Overview
Discovering that you’re pregnant is an exciting and joyous time, filled with planning and anticipation for your baby’s future. It can also be a time filled with questions and concerns — pregnancy leads to many changes in your body, as well as that of your growing fetus. With all of these changes, it’s important to stay healthy and work with your physician to find what works best for your individual pregnancy.
In this section, our experts provide general guidelines for staying healthy during pregnancy and what you can expect throughout your three trimesters.
The First Trimester
A healthy first trimester is crucial to your baby’s development. You may not be showing much on the outside yet, but on the inside, your baby’s major body organs and systems are forming.
- At your first prenatal visit, you will undergo a physical exam as well as certain tests and screenings to assess the health of you and your unborn baby.
- First trimester symptoms vary from woman to woman, with some experiencing all known symptoms and others only a few. Duration of symptoms can vary as well.
- After eight weeks, the embryo is referred to as a fetus.
- Although the fetus is only 1 to 1.5 inches long at this point, all major organs and systems have been formed.
- During the first trimester, the fetus is most susceptible to damage from substances, like alcohol, drugs and certain medicines, and illnesses, like rubella (German measles).
The Second Trimester
The second trimester marks a turning point for you and your baby. You will usually begin to feel better and start showing the pregnancy more. Your baby has developed all of its organs and systems, and will begin growing in length and weight.
- During your second trimester prenatal visits, your health care provider will continue to check on your and your baby’s health, including monitoring the fetal heartbeat.
- The second trimester is the most physically enjoyable for most women. Morning sickness usually lessens by this time, and the extreme tiredness and breast tenderness usually ease up.
- Your fetus has now developed all its organs and systems and will now begin to grow in length and weight.
- You may be able to feel the movement of the fetus for the first time at around 20 weeks. This phenomenon is called quickening.
- A fetus born at the end of 24 weeks may survive in a neonatal intensive care unit.
The Third Trimester
The third trimester marks the home stretch, as you prepare for the delivery of your baby. Your baby will continue to grow in length and weight.
- As you begin the third trimester, your health care provider or midwife may change the schedule of your prenatal visits from monthly to every two weeks.
- It’s a good idea to start taking childbirth classes in preparation for your baby’s birth, especially if this is your first pregnancy.
- By the end of the third trimester, the fetus is about 19 to 21 inches long and weighs, on average, 6 to 9 pounds.
Common Tests During Pregnancy
Your health care provider may recommend a variety of screenings, imaging techniques and tests throughout the three trimesters of your pregnancy.
- Genetic screening can help diagnose the potential for certain genetic disorders before birth.
- First trimester screening is a combination of fetal ultrasound and maternal blood testing. This screening process can help determine the risk of the fetus having certain birth defects.
- Second trimester prenatal screening may include several blood tests called multiple markers. These markers provide information about the risk of having a baby with certain genetic conditions or birth defects.
- You may have ultrasounds performed at different times in your pregnancy to check for fetal growth, estimate your due date and look for any structural abnormalities in the baby.
- Additional testing during pregnancy may include amniocentesis, chorionic villus sampling (CVS), fetal monitoring, glucose testing and Group B strep culture.
Nutrition During Pregnancy
It’s important to learn the best foods for a healthy pregnancy, what foods should be avoided, and the best vitamin and mineral supplements.
he Academy of Nutrition and Dietetics recommends the following key components of a healthy lifestyle during pregnancy:
Appropriate weight gain
A balanced diet
Regular exercise
Appropriate and timely vitamin and mineral supplementation
Dietary and Caloric Recommendations
To maintain a healthy pregnancy, approximately 300 extra calories are needed each day. These calories should come from a balanced diet of protein, fruits, vegetables and whole grains. Sweets and fats should be kept to a minimum. A healthy, well-balanced diet can also help to reduce some pregnancy symptoms, such as nausea and constipation.
Fluid Intake During Pregnancy
Fluid intake is also an important part of pregnancy nutrition. Follow these recommendations for fluid intake during pregnancy:
You can take in enough fluids by drinking several glasses of water each day, in addition to the fluids in juices and soups. Talk to your health care provider or midwife about restricting your intake of caffeine and artificial sweeteners.
Avoid all forms of alcohol.
Ideal Foods to Eat During Pregnancy

The following foods are beneficial to your health and fetal development during pregnancy:
Vegetables: carrots, sweet potatoes, pumpkin, spinach, cooked greens, tomatoes and red sweet peppers (for vitamin A and potassium)
Fruits: cantaloupe, honeydew, mangoes, prunes, bananas, apricots, oranges, and red or pink grapefruit (for potassium)
Dairy: fat-free or low-fat yogurt, skim or 1% milk, soymilk (for calcium, potassium, vitamins A and D)
Grains: ready-to-eat cereals/cooked cereals (for iron and folic acid)
Proteins: beans and peas; nuts and seeds; lean beef, lamb and pork; salmon, trout, herring, sardines and pollock
Foods to Avoid During Pregnancy
Avoid eating the following foods during pregnancy:
Unpasteurized milk and foods made with unpasteurized milk (soft cheeses, including feta, queso blanco and fresco, Camembert, brie or blue-veined cheeses—unless labeled “made with pasteurized milk”)
Hot dogs and luncheon meats (unless they are heated until steaming hot before serving)
Raw and undercooked seafood, eggs and meat. Do not eat sushi made with raw fish (cooked sushi is safe).
Refrigerated pâté and meat spreads
Refrigerated smoked seafood
Guidelines for Safe Food Handling
Follow these general food safety guidelines when handling and cooking food:
Wash. Rinse all raw produce thoroughly under running tap water before eating, cutting or cooking.
Clean. Wash your hands, knives, countertops and cutting boards after handling and preparing uncooked foods.
Cook. Cook beef, pork or poultry to a safe internal temperature verified by a food thermometer.
Chill. Promptly refrigerate all perishable food.
Prenatal Vitamin and Mineral Supplements
Most health care providers or midwives will prescribe a prenatal supplement before conception or shortly afterward to make sure that all of your nutritional needs are met. However, a prenatal supplement does not replace a healthy diet.
The Importance of Folic Acid
The U.S. Public Health Service recommends that all women of childbearing age consume 400 micrograms (0.4 mg) of folic acid each day. Folic acid is a nutrient found in:
Some green leafy vegetables
Most berries, nuts, beans, citrus fruits and fortified breakfast cereals
Some vitamin supplements.
Folic acid can help reduce the risk of neural tube defects, which are birth defects of the brain and spinal cord. Neural tube defects can lead to varying degrees of paralysis, incontinence and sometimes intellectual disability.
Folic acid is the most helpful during the first 28 days after conception, when most neural tube defects occur. Unfortunately, you may not realize that you are pregnant before 28 days. Therefore, your intake of folic acid should begin before conception and continue throughout your pregnancy. Your health care provider or midwife will recommend the appropriate amount of folic acid to meet your individual needs.
For example, women who take anti-epileptic drugs may need to take higher doses of folic acid to prevent neural tube defects. They should consult with their health care provider when considering trying to conceive.
Exercise During Pregnancy
Regular exercise, with the approval of your health care provider, can help reduce physical discomforts from pregnancy and help with postpartum recovery.
Medical Conditions and Pregnancy
There are certain medical conditions, whether pre-existing or those that develop during pregnancy, which may cause complications. Your health care provider will be able to help you manage these complications.
Care and Management of Multiple Pregnancy
Pregnancy with twins, triplets or higher-order multiples may necessitate different nutritional requirements and types of delivery.
Labor
Labor is a series of continuous, progressive contractions of the uterus that lead to the delivery of your baby.
Read more.
Delivery
Your baby may be delivered vaginally or by a cesarean section, depending on your baby’s position and other medical factors determined by your health care provider.
Delivery of the Baby
During delivery, your baby exits your body, followed by the placenta. In preparation for the delivery, you may be moved into a birthing or delivery room. You may also remain in the same room for both labor and delivery. Your partner is encouraged to be actively involved in the childbirth process by helping you with relaxation methods and breathing exercises.
Positions for delivery may vary, ranging from squatting or sitting positions to semiseated positions. In a semiseated position, you are partially lying down and partially sitting up, allowing gravity to help you push the baby through the birth canal. Your delivery position depends on your preference, the recommendation from your health care provider and the health of your fetus.
During the delivery process, medical personnel will continue monitoring your vital signs, including blood pressure and pulse, and the fetal heart rate. Your health care provider will examine your cervical opening to determine the position of your baby’s head and continue to support and guide you in your efforts to push.
Delivery can be done either vaginally or by C-section.
Vaginal Delivery
During a vaginal delivery, your health care provider will assist the baby’s head and chin out of the vagina when it becomes visible. Once the head is delivered, your health care provider will apply gentle downward traction on the head to deliver the shoulders, followed by the rest of the body. The baby turns itself as the last movement of labor.
In some cases, the vaginal opening does not stretch enough to accommodate the fetus. If the baby is in distress, it may be necessary to accelerate delivery using an episiotomy. During this procedure, the doctor cuts the vaginal wall and the perineum (area between the thighs, extending from the anus to the vaginal opening) to help deliver the baby. Episiotomies are not needed for every delivery and are not performed routinely.
After the delivery of your baby, you will be asked to continue to push during the next few uterine contractions to deliver the placenta. This process may take up to 30 minutes. Once the placenta is delivered, any tear or episiotomy cut is repaired. Your health care provider will likely give you oxytocin to help contract the uterus. This drug will be injected into your muscles or delivered intravenously. The uterus is then massaged to further help it contract and to help prevent excessive bleeding. Some bleeding is normal and should be expected following a vaginal delivery.
Cesarean Section
If you’re unable to deliver your baby vaginally, your baby will be delivered by a C-section. This surgical procedure is usually performed in an operating room or a designated delivery room. Some C-sections are planned and scheduled, while others may be performed as a result of complications that occur during labor.
Once the anesthesia has taken effect, the physician will make a cut in the abdomen and create an opening in the uterus. After the amniotic sac is opened, the baby is delivered through the opening. During the procedure, you may feel some pressure and/or a pulling sensation.
Following the delivery of your baby, your health care provider will stitch up your uterus and the cut that was made in your abdomen. After a C-section, you may still experience some vaginal bleeding.
Conditions for a C-Section
Several conditions may increase your chance of delivering via C-section, including:
Abnormal delivery presentation
A previous C-section
Fetal distress
Labor that fails to progress or progresses abnormally
Placental complications, such as placenta previa (the placenta blocks the cervix, which could cause the placenta to prematurely detach from the uterus)
Twins, triplets and higher-order multiple gestations
Possible Labor and Delivery Complications
Although serious complications are rare during labor, the most common complications include:
Fetal Meconium
When the amniotic sac ruptures, the normal color of the amniotic fluid is clear. If the amniotic fluid is green or brown in color, it may indicate fetal meconium, which is normally passed after birth as the baby’s first bowel movement. Meconium in the amniotic fluid may be associated with fetal distress.
Abnormal Fetal Heart Rate
The fetal heart rate helps indicate how well your baby is handling the contractions. This vital sign is usually monitored electronically during labor. The normal range is between 120 and 160 beats per minute.
If your baby appears to be in distress, your health care provider may take immediate action to stabilize your baby’s heart rate. You may be given oxygen, an increase in intravenous fluids or a new labor position.
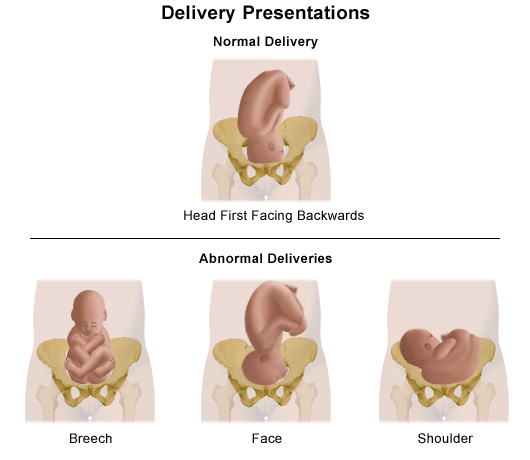
Abnormal Fetal Positions During Delivery
The normal position for your baby during birth is head down, facing your back. If your baby is not in this position, it can make delivery through the birth canal more difficult. The following are the most common abnormal fetal delivery positions:
Head down but facing your front
Face down in your pelvis (instead of the top of the fetal head)
Brow down in your pelvis
Breech (buttocks or feet are down first in your pelvis)
A shoulder or arm in your pelvis
Depending on the position, your health care provider may try to deliver the fetus as it presents itself, attempt to turn the fetus before delivery or perform a C-section.