Sleep Better
Most people have trouble sleeping from time to time because of travel, changes in schedule or lifestyle or stressful situations throughout the day. Lack of sleep can affect emotional and physical health.
There are many tips for how to get enough sleep that don’t involve medication or seeing a sleep specialist. Diet modifications, yoga, reducing screen time before bed and bedroom preparation are all important factors in getting to and staying asleep.
The Science of Sleep: Understanding What Happens When You Sleep
Sleep accounts for one-quarter to one-third of the human lifespan. But what exactly happens when you sleep?

Before the 1950s, most people believed sleep was a passive activity during which the body and brain were dormant. “But it turns out that sleep is a period during which the brain is engaged in a number of activities necessary to life. Researchers are spending many of their waking hours trying to learn more about these processes and how they affect mental and physical health. Here is a glimpse into the powerful (often surprising) findings of sleep researchers—and what they’re still trying to discover about the science of sleep.
All Sleep Is Not the Same
Throughout your time asleep, your brain will cycle repeatedly through two different types of sleep: REM (rapid-eye movement) sleep and non-REM sleep.
The first part of the cycle is non-REM sleep, which is composed of four stages. The first stage comes between being awake and falling asleep. The second is light sleep, when heart rate and breathing regulate and body temperature drops. The third and fourth stages are deep sleep. Though REM sleep was previously believed to be the most important sleep phase for learning and memory, newer data suggests that non-REM sleep is more important for these tasks, as well as being the more restful and restorative phase of sleep.
As you cycle into REM sleep, the eyes move rapidly behind closed lids, and brain waves are similar to those during wakefulness. Breath rate increases and the body becomes temporarily paralyzed as we dream.
The cycle then repeats itself, but with each cycle you spend less time in the deeper stages three and four of sleep and more time in REM sleep. On a typical night, you’ll cycle through four or five times.
Research Shows Your Genes Affect Your Sleep Clock
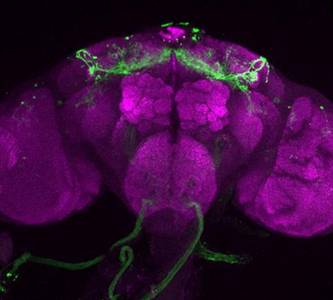
fellow researchers recently identified a gene involved in the circadian regulation of sleep timing. When researchers removed this gene—called “wide awake”—from fruit flies, the flies experienced problems falling asleep and staying asleep. A similar sleep gene exists in both humans and mice. Scientists continue to study this gene in hopes of understanding more about how processes within our cells affect our ability to sleep.
Your Body’s Built-In Sleep Controls
According to researchers, there are two main processes that regulate sleep: circadian rhythms and sleep drive.
Circadian rhythms are controlled by a biological clock located in the brain. One key function of this clock is responding to light cues, ramping up production of the hormone melatonin at night, then switching it off when it senses light. People with total blindness often have trouble sleeping because they are unable to detect and respond to these light cues.
Sleep drive also plays a key role: Your body craves sleep, much like it hungers for food. Throughout the day, your desire for sleep builds, and when it reaches a certain point, you need to sleep. A major difference between sleep and hunger: Your body can’t force you to eat when you’re hungry, but when you’re tired, it can put you to sleep, even if you’re in a meeting or behind the wheel of a car. When you’re exhausted, your body is even able to engage in microsleep episodes of one or two seconds while your eyes are open. Napping for more than 30 minutes later in the day can throw off your night’s sleep by decreasing your body’s sleep drive.
Why You Need Sleep
If you have ever felt foggy after a poor night’s sleep, it won’t surprise you that sleep significantly impacts brain function. First, a healthy amount of sleep is vital for “brain plasticity,” or the brain’s ability to adapt to input. If we sleep too little, we become unable to process what we’ve learned during the day and we have more trouble remembering it in the future. Researchers also believe that sleep may promote the removal of waste products from brain cells—something that seems to occur less efficiently when the brain is awake.
Sleep is vital to the rest of the body too. When people don’t get enough sleep, their health risks rise. Symptoms of depression, seizures, high blood pressure and migraines worsen. Immunity is compromised, increasing the likelihood of illness and infection. Sleep also plays a role in metabolism: Even one night of missed sleep can create a prediabetic state in an otherwise healthy person. “There are many important connections between health and sleep,” says Wu.
Melatonin for Sleep: Does It Work?
Melatonin sleep aids are growing in popularity, with 3 million Americans using them in 2012, according to a nationwide survey from the Centers for Disease Control and Prevention. If you’re among them or are considering melatonin for sleep, it’s smart to understand exactly how melatonin works.

“Your body produces melatonin naturally. It doesn’t make you sleep, but as melatonin levels rise in the evening it puts you into a state of quiet wakefulness that helps promote sleep,”
“Most people’s bodies produce enough melatonin for sleep on their own. However, there are steps you can take to make the most of your natural melatonin production, or you can try a supplement on a short-term basis if you’re experiencing insomnia, want to overcome jet lag, or are a night owl who needs to get to bed earlier and wake up earlier, such as for work or school.”
If you’d like to harness melatonin’s sleep-inducing effects, Buenaver recommends taking these steps.
Work with, not against, melatonin’s sleep-inducing signals.
“Melatonin levels rise about two hours before bedtime,” Buenaver says. “Create optimal conditions for it to do its job by keeping the lights low before bed. Stop using your computer, smartphone or tablet—the blue and green light from these devices can neutralize melatonin’s effects. If you watch television, be sure you’re at least six feet away from the screen. Turn off bright overhead lights too.” Meanwhile you can help program your body to produce melatonin for sleep at the right time of day by getting exposure to daylight during the morning and afternoon. Take a walk outside or sit beside a sunny window.

Consider melatonin sleep help for occasional insomnia.
“Even sound sleepers have trouble falling asleep or staying asleep once in a while,” Buenaver says. “You may want to try melatonin for sleep if you have difficulty for more than a night or two.” Research shows that a supplement may help people with insomnia fall asleep slightly faster and may have bigger benefits for those with delayed sleep phase syndrome—falling asleep very late and waking up late the next day.
Use melatonin sleep supplements wisely and safely.
“Less is more,” Buenaver says. Take 1 to 3 milligrams two hours before bedtime. To ease jet lag, try taking melatonin two hours before your bedtime at your destination, starting a few days before your trip. “You can also adjust your sleep-wake schedule to be in sync with your new time zone by simply staying awake when you reach your destination—delaying sleep until your usual bedtime in the new time zone. Also, get outside for natural light exposure. That’s what I do,” Buenaver says.
Know when to stop.
“If melatonin for sleep isn’t helping after a week or two, stop using it,” says Buenaver. “And if your sleep problems continue, talk with your health care provider. If melatonin does seem to help, it’s safe for most people to take nightly for one to two months. “After that, stop and see how your sleep is,” he suggests. “Be sure you’re also relaxing before bed, keeping the lights low and sleeping in a cool, dark, comfortable bedroom for optimal results.”
Skip melatonin for sleep if …
Do not use melatonin if you are pregnant or breastfeeding or have an autoimmune disorder, a seizure disorder or depression. Talk to your health care provider if you have diabetes or high blood pressure. Melatonin supplements may also raise blood-sugar levels and increase blood pressure levels in people taking some hypertension medications.
Sleep Problems: Look for Health Connections
A wide variety of health issues (as well as the medications that treat them) can have a surprising connection to the quality of your sleep. Here’s how some common conditions are linked with sleep problems:

Allergies: Allergies to dust mites, mold, pollen and other substances cause sneezing, congestion and itchy, watery eyes that can lead to more nighttime wakeups and poor sleep quality. “If you have mild obstructive sleep apnea (pauses in breathing), a stuffed-up nose could make it worse because you will have to breathe through your mouth more often,”. Meanwhile, allergy medicines containing pseudoephedrine can keep you from falling asleep while those containing antihistamines such as diphenhydramine can leave you feeling extremely drowsy the following day.
Alzheimer’s disease: Insomnia and daytime sleeping are more common in the later stages of Alzheimer’s disease . Maintaining a regular daytime schedule and, if needed, medications can help sleep quality.
Asthma: For about 60 percent of people with asthma, airway changes at night (called “nocturnal asthma”) can lead to coughing, wheezing and breathlessness that interrupt sleep. The asthma drug theophylline can contribute to sleep problems and more frequent nighttime awakenings, as can using the quick-relief inhaler drug albuterol more often than your doctor recommends.
Benign prostatic hyperplasia: Up to 14 million American men have an enlarged prostate gland; as a result, nearly one in three men older than age 60 wake up two or more times each night to use the bathroom. Medications can help.
Chronic obstructive pulmonary disease (COPD): Lung disorders such as emphysema, chronic bronchitis and asthma can lead to coughing, chest pain and difficulty breathing that compromises sleep quality for nearly 50 percent of the more than 12 million Americans with COPD . Oxygen levels in your blood may drop, causing daytime tiredness. In addition, up to 15 percent of people with COPD may have sleep apnea. Some COPD medications such as albuterol and prednisone can also bring on sleep problems.
Congestive heart failure: More than five million Americans have congestive heart failure , which weakens the heart’s ability to pump and also increases your risk of sleep apnea and sleep-disrupting shaking of the arms and legs called periodic limb movements. Treatments for heart failure can help; you may also need apnea treatments such as a continuous positive airway pressure breathing machine.
Depression and anxiety: “Everyone has a bad night of sleep once in a while, perhaps because you’re stressed or worried about an event in your life. But if sleep problems persist, depression or anxiety could be involved,“ Treating depression and anxiety can help your sleep quality, and treating sleep problems can improve these mental-health issues. You and your doctor may have to look at both.”
Diabetes: High blood sugar levels can prompt your kidneys to excrete more glucose into your urine, leading to more nighttime bathroom trips. In addition, many people with diabetes are also overweight, which can raise your risk of sleep apnea. Pain from diabetes-related nerve damage (peripheral neuropathy) and night sweats due to shifting blood sugar levels may affect your sleep quality too.
Gastroesophageal reflux: Studies show that as many as three out of four people with heartburn have night symptoms at least once a week. Lying down worsens the painful backwash of stomach acid into the esophagus. Avoiding large meals and alcohol before bed and raising the head of your bed about six inches may help.
Parkinson’s disease: Insomnia, nightmares, acting out dreams during sleep, sleep apnea and falling asleep without warning during the day are among the sleep problems that people with Parkinson’s disease may experience. Medications may help, though some Parkinson’s disease drugs can contribute to insomnia; your doctor may suggest taking them earlier in the day.
Sleepless Nights? Try Stress Relief Techniques
In a recent national survey, 44 percent of adults said stress had caused sleepless nights at least once in the previous month. All that tossing, turning and staring at the ceiling can leave you feeling tired and more stressed the next day. If you’re caught in this vicious cycle of anxiety and insomnia, there’s good news: Simple stress relief techniques can help you sleep better and feel calmer.
.ashx?h=357&iar=0&mh=360&mw=520&w=520&hash=EE18E273F380311B4168007DEA409821)
Understanding Anxiety and Insomnia
What’s behind the more stress, less sleep connection? “If you’re frequently triggering your stress response, your body never gets back to its baseline,”
“Stress and sleepless nights are closely linked,”. “If you’re in pain, tend to worry, or are coping with a difficult situation in your life, you may have more stress hormones than usual circulating in your body. A poor night’s sleep adds even more. And those hormones may never be fully broken down. It’s like running an engine in fifth gear all the time.”
Try It Activate Your Body’s Relaxation Response
“We recommend planned relaxation activities to reduce stress. Watching a ballgame or movie on TV just isn’t the same as taking the time to fully relax,” Try this plan:
1. Practice gentle breathing and progressive muscle relaxation every day (20 to 25 minutes) for two weeks. On a scale of 0 (“totally relaxed”) to 10 (“completely tense”), rate your level of emotional and physical stress before and after.
2. After two weeks, choose the exercise that works best for your anxiety and insomnia and keep it up every day. “With practice, your body and mind will learn to relax more quickly and deeply for fewer sleepless nights”.
Stress Relief Techniques to the Rescue
“Activities that switch on the body’s natural relaxation response feel great. “And they have been proven by research to improve sleep. They help by reducing the release of the stress hormones cortisol and adrenaline and by slowing your heart rate and breathing. Your body and mind calm down.”
Yoga, tai chi, herbal treatment and meditation are helpful stress relief techniques. So are these two simple exercises that are recommends to patients who are struggling with sleepless nights.
Gentle breathing:
- In a quiet place, sit or lie down in a comfortable position. It may help to close your eyes.
- Breathe slowly in and out for about five minutes. As you inhale, breathe down into your belly. Focus on your breath.
- If you’d like, repeat to yourself, “Breathing in I am calm, breathing out I am coping.”
Progressive muscle relaxation:
- In a quiet place, sit or lie down in a comfortable position.
- Take a few gentle breaths, in and out.
- Begin tensing groups of muscles one at a time as you breathe. Hold the tension as you inhale, then release it as you exhale. Take a few breaths as you notice (and enjoy) how relaxed each muscle group feels.
- Start with the muscles in your head, neck and face. Move down to your shoulders, hands and arms, back, stomach, buttocks, thighs, calves and feet.
- Repeat for any areas that are still tense.
“As you go through this exercise, feel the presence and absence of tension so you can spot lingering tension and do something about it.
Insomnia
What is insomnia?
Insomnia, which means difficulty initiating or maintaining sleep, is a symptom, not a diagnosis or a disease. It may be due to a lack of sleep or poor quality of sleep.
You’ve probably had nights when you couldn’t fall asleep, no matter how desperately you tried.
When you can’t sleep, the ticking of the clock only reminds you of your exhaustion and the endless hours until morning. And perhaps you finally drop off around dawn, only to be jarred awake by the alarm an hour later.
Insomnia is one of the most common sleep complaints. About 1 in 3 adults has bouts of insomnia that last a few days at a time. This is acute insomnia. But 1 in 10 adults suffers ongoing difficulty sleeping, known as chronic insomnia. This is defined as insomnia that occurs more than 3 nights a week for over a month.
Insomnia affects people in different ways. If you suffer from it, you may not be able to go to sleep or you may not be able to stay asleep. You might constantly wake up earlier than you would like, perhaps in the wee hours of the morning, and find yourself unable to go back to sleep.
Women are more likely to have insomnia than men. It is also more common among shift workers, who don’t have consistent sleep schedules; people with low incomes; people who have a history of depression; and those who don’t get much physical activity.

Seven Ways to Get a Healthier Night’s Sleep
Around 18 million Americans fail to get a good night’s sleep.If you or someone you love is among them, these research findings and expert insights could help you figure out what’s holding you back and what can help.
What causes insomnia?
Insomnia has many possible causes. The reasons you’re lying awake when you don’t want to be are individual. They can include any or all of these:
Medications that interfere with sleep
Dietary choices, such as caffeine late in the day, that interfere with sleep
Stressful thoughts
Depression
Recent upheavals in your life, such as a divorce or death of a loved one
Hormone changes, such as those accompanying menopause
Bedtime habits that don’t lead to restful sleep
Sleep disorders
Chronic pain
Medical conditions such as acid reflux, thyroid problems, stroke, or asthma
Substances like alcohol and nicotine
Travel, especially between time zones
What are the symptoms of insomnia?
These are common symptoms of insomnia:
Frustration and preoccupation with your lack of sleep
Physical aches and pains, such as headaches and stomachaches
Impaired performance at work
Daytime drowsiness or low energy
Difficulty paying attention
Anxiety
Tension and irritability
Depression and mood swings
How is insomnia diagnosed?
You may need to see a sleep medicine specialist to find out what’s causing your insomnia. It will be helpful to bring a record of your sleep patterns.
The process of making a diagnosis may include:
Your medical history. Your doctor will consider any medical conditions, any medications you’re taking, and stressful life changes that could be causing insomnia.
Your sleep history. Be prepared to describe your insomnia with details such as how long it’s been going on, what you think could be contributing to it, and what your sleep is like, such as whether you can barely get to sleep at all or if you wake up too early.
Physical exam. The doctor will look for any physical reasons that could be causing sleep problems.
Sleep study. You may need to sleep overnight in a sleep lab where researchers monitor your sleep.
Diagnosis of insomnia begins with a good medical history. The physician will seek to identify any medical or psychological illness that may be contributing to the patient’s insomnia, as well as screen for drug and alcohol use. The patient may be asked about chronic snoring and recent weight gain, which may lead to the possibility of obstructive sleep apnea. In such cases the doctor may request an overnight sleep test, or polysomnogram, though sleep studies are not part of the routine initial workup for insomnia. Patients may also be asked to keep a daily diary of their alertness
How is insomnia treated?
You have many options for treatment:
Medications to help you get to sleep and stay asleepHerbal treatment from Dr Eboka Herbal Remedies
Change in existing medication if that’s what’s causing the problem
Counseling to help relieve stress and other issues bothering you
Change in lifestyle choices that may interfere with sleep
Insomnia generally resolves itself when the underlying medical or psychiatric cause is removed. Treating the symptoms of insomnia without addressing the main cause is rarely successful. Most people seek medical attention when their insomnia becomes chronic. Therapies include both nonpharmacologic and pharmacologic treatments. Studies have shown that combining medical and nonmedical treatments typically is more successful in treating insomnia than either one alone.
What are the complications of insomnia?
Insomnia can have serious complications. Poor sleep quality is linked to:
Increased risk for heart disease
Increased risk for stroke
Increased risk for diabetes
Excessive weight gain or obesity
Depression
Increased risk for injury to yourself or others, such as a car accident caused by driving while drowsy
Key points
Insomnia, the term for having trouble sleeping at night, is one of the most common sleep complaints. About 1 in 3 adults has bouts of insomnia that last a few days at a time. Women are more likely to have insomnia than men.
Insomnia has many possible causes. You may need to see a sleep medicine specialist to find out what’s causing your insomnia.
Common symptoms of insomnia include impaired work performance, daytime drowsiness or low energy, difficulty: paying attention and others.
Diagnosis may involve a sleep study in which a sleep specialist monitors your sleep.
Next steps
Tips to help you get the most from a visit to your health care provider:
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your provider tells you.
At the visit, write down the names of new medicines, treatments, or tests, and any new instructions your provider gives you.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your provider if you have questions.
